Before discussing the tests, we need to cover a few definitions:
- T3 (triiodothyronine) – this is the active thyroid hormone.
- rT3 (reverse T3) – an inactive form of T3 that blocks active T3 from reaching its receptors
- T4 (thyroxine) – this is the pro-hormone that is converted to the active hormone T3.
- TSH (thyroid stimulating hormone – aka thyrotropin) – this is the hormone that is released by the pituitary and tells the thyroid gland to make more hormone (mostly T4) and does so when T4 levels are low.
- TBG (thyroid binding globulin) – a protein that the majority of both circulating T4 & T3 bind to in the blood
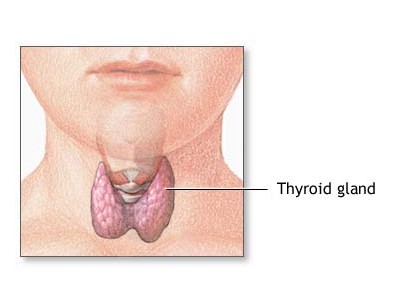
For more details on how the thyroid gland and hormones work go to Thyroid Function
What Are The Tests Used To Measure Thyroid Function?
Historically, around the turn of the century, cholesterol blood levels were used to determine if someone was hypothyroid. If your cholesterol levels were high, you were considered hypothyroid and given thyroid replacement hormone until they were brought down to normal. This method was used into the mid-century. The BMR (basal metabolic rate), used in the 30s – 40s required a BMR machine to measure but was hampered by difficulties. Radioactive iodine uptake by the thyroid was considered the most accurate test in the 50s – 60s after it became available from the Tennessee Valley Atomic Energy Complex. In the 60s this was supplanted by the PBI (protein bound iodide) test when the Radioactive iodine uptake test lost its luster. Then total T4 became the “gold standard”, eventually to be displaced by TSH commonly used as “The One” test today.
The most common test is TSH, a blood test that is used routinely by your doctor to screen for thyroid dysfunction, if you have symptoms of hypothyroidism. As you can see from the information above, TSH is not the active hormone. It stimulates production of T4, which must then be converted to T3 to become the active hormone. The amount of TSH is primarily under the control of T4 levels. When T4 is high, TSH is low and when T4 is low, TSH is high. So, your doctor looks to see if your TSH is high and if it is then tells you you are hypothyroid. All other hormones our bodies make are measured directly (i.e. estrogen, testosterone, cortisol…). Thyroid is the only one measured 2 full stages away from the actual hormone i.e measuring TSH instead of T3.
The “normal” range for TSH from 1970 to 1985 was considered to be less than or equal to 10mIU/L. From 1985 to 1990 the range went from 0.35 to 5.5 and from 1990 to the present the range is 0.35 to 4.5. However, in 2002, the National Academy of Clinical Biochemistry (NACB) released new guidelines stating that when more sensitive screening was done “normal” TSH was between .4 and 2.5. And in January 2003, the American Association of Clinical Endocrinologists backed NACB’s guidelines, saying doctors should “consider treatment for patients who test outside the boundaries of a narrower margin based on a target TSH level of .3 to 3.0.”
How did they determine this new “normal” range? What did they mean by “more sensitive screening”? They “excluded people with thyroid disease” – people who were hypothyroid but were undiagnosed! How did that happen? Doctors were using the “normal” values for TSH to base their diagnosis on and not patient’s symptoms! What range are labs using for their normal levels at the present time 10 years after these recommendations were made? 0.35 to 4.5, leaving many people with hypothyroidism undiagnosed!
So, you can see that if your TSH was 7.0 in 1972 you weren’t considered to be hypothyroid, but in 1992 you would be. And if your TSH is 3.2 your doctor will most likely say you are “normal” even though you have symptoms and the most appropriate reference range only goes up to 2.5! There are also other irregularities concerning this number that make it less than reassuring for making the diagnosis of hypothyroidism. Three of these irregularities are seen in Hashimoto’s Thyroiditis, Subclinical Hypothyroidism and Low T3 Syndrome.
- Total T4 is a measure of the total amount of T4 circulating in the blood. This is both T4 bound to TBG and Free T4, which is unbound.
- Free T4 is unbound and therefore available to the tissues for conversion to T3 (the active hormone).
- Total T3 is the total of T3 bound to TBG and unbound (free) T3.
- Free T3 is unbound T3 available to the tissues for direct action.
- Reverse T3 (rT3) is an inactive form of T3. An enzyme called deiodinase converts T4 to T3 There are several of these enzymes. One of these converts T4 to rT3. Under conditions of stress, illness or aging, more T4 gets converted to rT3. This not only decreases T3 but also rT3 blocks the T3 receptor.
- Thyroperoxidase Antibody (TPOAb) – Under conditions of Leaky Gut (Intestinal Permeability Syndrome), autoimmune diseases can develop. Gluten sensitivity is the most well known cause of this. One of the common autoimmune diseases to develop under these conditions is Hashimoto’s Thyroiditis in which TPOAb is the most common autoantibody. This can cause hypothyroidism symptoms even when the other measures of thyroid function appear normal.
- Anti-Thyroglobulin Antibody (TGAb) – Thyroglobulin is a protein used in the thyroid gland to make thyroid hormone. In Hashimoto’s Thyroiditis, this antibody may also be found.
- Ferritin, Iron, Total Iron Binding Capacity (TIBC) & % Saturation – These are all different measures of Iron; both intracellular & circulating (bound & free). Iron is extremely important in the proper conversion of T4 to T3.
- Selenium – Used by the enzyme Deiodinase to convert T4 to T3.
- Zinc – Used by the thyroid gland to make T4.
- TBG is rarely measured but under certain conditions can be important as its level can be affected by estrogen, cortisol & liver disease.
What are the best measures?
The best measures of Thyroid Hormone Function are free T3 & free T4. This tells you how much of the active hormone, T3 is available to the tissues. T3 has a short existence (half-life) and so having a ready supply of T4 available is very important because it has a much longer half-life. TSH may be ordered as well, and may add some value in the diagnosis of “Subclinical Hypothyroidism”. In addition, it is important to measure for the TPOAb and TGAb (anti-thyroid antibodies) to make the diagnose Hashimoto’s Thyroiditis, if it is present. This is very important, because it indicates the presence of Intestinal Permeability Syndrome, which can lead to other autoimmune disease and cancer and is reversible and preventable. Reverse T3 is helpful in “Low T3 Syndrome” and if symptoms and lab tests don’t add up. Most doctors only order TSH or other tests whose value are questionable.
If my Dr. says my “thyroid hormone levels are normal” does this mean I’m not hypothyroid even when I have the symptoms?
“If you listen to your patients long enough, they will tell you what they have!” These were the words of one of our medical school professors who taught medical diagnosis. This is the cornerstone of “clinical diagnosis”! Clinical diagnosis is the diagnosis that is made based on the history and physical – the story that the patient presents to you in symptoms and signs (findings on physical exam). So, if you are the patient and you have the symptoms and signs of hypothyroidism, then you are clinically hypothyroid. The clinical diagnosis is made. Then your blood tests are evaluated to see if they confirm the diagnosis. With clinical hypothyroidism the blood tests may not confirm the clinical diagnosis, but that does not mean you don’t have hypothyroidism.
Here’s why:
Your genes code for proteins – structural proteins that make up bone & connective tissue, enzymes that direct all metabolic biochemical reactions in your cells, signaling molecules (hormones) and their receptors. If there is a genetic mutation in the gene that codes for your thyroid receptors that means they will not function as well. If that is the case you could have normal thyroid hormone levels, but your receptors would not respond as well and you would have symptoms of hypothyroidism. This is called thyroid resistance. Researchers are finding more and more cases of this.
That is not to say that thyroid resistance is the only reason for someone to have symptoms of hypothyroidism and yet have “normal” levels of thyroid hormone. Remember above when they switched the upper “normal” range for TSH from 5 to 2.5 because someone decided that they were including a lot of hypothyroid patients in the “normal” category? What’s to say that isn’t still going on? And even though using the new upper limit of 2.5 for TSH has been recommended by the National Academy of Clinical Biochemistry and 3.0 by the American Association of Clinical Endocrinologists, labs are still using 4.5 as the upper limit!
Bottom Line: If you feel like you’re hypothyroid and you look like you’re hypothyroid, you’re probably hypothyroid!
You may also want to read the articles: “Am I Hypothyroid?”, “Signs & Symptoms of Hypothyroidism”, “Signs and Symptoms of Hyperthyroidism” and “Thyroid Function”. If you wish to fill out a questionnaire to see if you may have a thyroid disorder, please download and complete the Hypothyroid Risk Questionnaire, and email it back to [email protected]. If you have any questions, please call us at 727-202-6807.



0 Comments