.
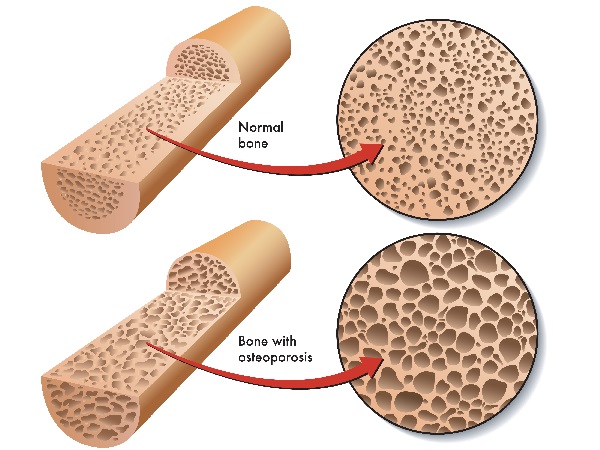
What is osteoporosis? To be honest, this is not really an easy question, though you will hear simple answers from many practitioners. “It is thinning of the bones.” “It is low bone mineral density (BMD).” ”It is loss of calcium in the bones.” ”It increases your risk of fracture.” All of these statements may be true, but they don’t tell the cause of osteoporosis, which is the important question. Your practitioner may have told you to just take calcium or calcium & vitamin D or may have put you on a medication to increase your bone density. These still don’t answer, “What causes osteoporosis?”
It may come as a surprise to many, but it is not a deficiency of calcium intake. Studies actually show that supplementation with calcium alone does not reduce the risk of fracture in patients with osteoporosis or osteopenia (a milder form of decreased BMD). Research also shows that supplementing with vitamin D plus calcium does no better than supplementing with vitamin D alone. When taken together these 2 pieces of information mean that calcium does nothing to treat or prevent Osteoporosis. Yes that is correct; calcium supplementation does not prevent fractures associated with Osteoporosis. What does this mean? It means that calcium deficiency is not the cause and therefor calcium supplementation is not the solution. As a matter of fact in a 2013 study of 61,433 women, those with the highest intake of calcium, including those who supplemented calcium had an all-cause mortality rate of 2.5 times greater than the women who did not supplement calcium. So not only does calcium supplementation not correct osteoporosis, but it increases your risk of dying by 250% according to this study. Other studies also show that calcium channel blocking nutraceuticals and pharmaceuticals decrease all-cause mortality. So supplementing with calcium is actually bad for you and does nothing to prevent or treat Osteoporosis.
So, if insufficient dietary calcium intake isn’t the cause of osteoporosis, what is? To answer that we need to look at bone formation – what stimulates it to form and what stimulates it to reabsorb. Our bones are undergoing “remodeling” all the time. Old bone gets reabsorbed and new bone forms continuously.
Let’s first look at bone formation. You have cells called osteoblasts that form bone by making collagen, which requires vitamin C. Collagen is a protein that is the basis of all the connective tissue in your body, including bone. Collagen is very tough and is held together by cross-linking between collagen molecules. This forms a lattice or matrix. Your osteoblasts also make osteopontin – a different kind of protein that forms powerful cross-bridges throughout the collagen matrix. Osteopontin has many negatively charged amino acids that combine with calcium which is positively charged. Osteocalcin is also produced by your osteoblasts which increases the number of positively charged calcium ions which then deposit onto your osteopontin. This is how your body forms bone. Pretty cool, right?
Bone reabsorption occurs as the result of other cells called osteoclasts producing and releasing collagenase and acid onto bone. Collagenase is an enzyme that digests (breaks down) collagen and the acid causes calcium to ionize and leach from (leave) bone.
Osteoporosis (& Osteopenia) occurs when there is more bone resorption than bone formation. The things that stimulate bone formation and inhibit bone resorption prevent Osteoporosis. Let’s look at these:
Magnesium increases bone density and decreases fracture risk, is a calcium channel blocker (CCB) and decreases all-cause mortality.
Vitamin K increases quality of bone and reduces bone fracture risk, decreases all-cause mortality and helps prevent coronary artery calcification.
Vitamin C decreases bone resorption and increases bone synthesis, increases bone mineral density, decreases fracture risk, increases fracture healing, reduces inflammation and decreases all-cause mortality.
Vitamin D along with a diet sufficient in vegetables and fruits assures adequate calcium absorption, is a key determinant of bone mineral density, is vital for immune function and decreases all-cause mortality. Blood levels above 60 are associated with risk reduction for multiple diseases including auto-immune & cancer.
Essential fatty acids protect against bone mineral density loss, are CCBs, and decreases all-cause mortality.
Estrogen decreases osteoporosis and osteoporotic fractures, decreases inflammatory cytokines, decreases coronary artery calcification and decreases all-cause mortality.
Testosterone significantly decreases osteoporotic fracture risk, reduces coronary artery calcification, is a CCB, is a coronary artery dilator and decreases all-cause mortality
Thyroid hormone is necessary for bone mass development and attaining peak bone mass. Optimal levels decrease the risk of osteoporotic fracture all-cause mortality.
There are other factors that are important: eating a healthy diet rich in leafy greens vegetables & fruits, exercising effectively and reducing your exposure to toxins. Detoxify regularly. Take a good multivitamin. Inflammation and oxidative stress increase bone reabsorption so get your markers of inflammation and oxidative stress tested. Acidity (not stomach) increases bone resorption so drink water with lime or lemon juice. Additional minerals that help build bone are Boron, Manganese, Silicon & Zinc (but too much zinc can cause bone resorption)
Risk factors for Osteoporosis – Below is a list of those conditions that increase your risk of Osteoporosis. If you have any of these it is a good idea to be evaluated for them and to correct the underlying conditions (bring the body back into balance) as they will not only increase risk for Osteoporosis, but may often lead to other chronic problem.
- Menopause/Andropause
- Hyperthyroidism
- Hyperparathyroidism
- Vitamin Deficiency
- Relative vitamin C deficiency
- Relative magnesium deficiency
- Relative vitamin K deficiency
- Essential fatty acid deficiency
- Inflammation
- Oxidative stress
- Stress – high levels of cortisol
- Excessive protein intake
- Smoking
- Alcohol abuse
- Genetic predisposition
- Fair complexion
- Thin bone structure
- No menstrual cycle for > 6 months
- Lack of exercise
- Fluoride
- High fat diet
- Excess zinc supplementation
- Excessive vitamin A supplementation
- Acidifiers – soda, carbonated water, coffee, etc.
- Soda has 2 problems
- CO2 combines with water to make acid
- Phosphate leaches calcium
- Coffee
- Is acidic
- Caffeine causes calcium loss
- > 1,000 OTC medications contain caffeine
- Medications
- Anticonvulsants
- Corticosteroids
- Heparin
- Isoniazide
- Lasix
- Lithium
- Methotrexate
- Tetracycline
- SSRI antidepressants
- PPI antacids
- Surgery
- Disease States
- Kidney disease
- Rheumatoid Arthritis
- COPD
- Multiple myeloma
- Scoliosis
- Anorexia nervosa
- Diabetes mellitus
- Cushing’s disease
- Pyercalciuria
- Gallbladder disease
- Primary biliary cirrhosis
- Fat malabsorption
- Hypochlorhydria
- Lactose intolerance
- History of chronic low back pain > 10 years
- History of stress fracture
- Women who have never had the extended exposure to high estrogen levels of pregnancy
- Soda has 2 problems
Call our office 727-202-6807 to schedule an appointment for evaluation and treatment of your bone health.



0 Comments