If you have Type 2 Diabetes (T2D), you’ve probably seen a doctor and been put on a blood sugar lowering medication (such as metformin) for it. If you asked how you got it, you may not have gotten an answer, other than been told to diet, lose weight and exercise. If you’ve tried these but failed, it may not be your fault. You simply may not have had enough information. So let’s start at the beginning with how our body’s cells normally work and then how T2D begins. (This information does not apply to Type 1 Diabetes, which occurs for totally different reasons.)
Normally, your cells use glucose for energy. Glucose is the end product of 90+% of all the sugar and non-fibrous carbohydrates you eat. Muscle and heart cells also use fat for energy, but your brain can only use glucose for energy (with one dietary exception). This total requirement of your brain for glucose means that if your glucose drops too low, you’re in trouble – you can become unconscious and even die. So, it is very important for your blood glucose (aka Blood Sugar or BS) level not to drop too low – generally not below 50. Thankfully your body is exceedingly good at preventing this. It has 5 hormones that prevent this from happening – Glucagon, Adrenaline, Norepinephrine, Cortisol and Growth hormone. These 5 hormones are called Counter-Regulatory Hormones because they counter the effects of the single hormone that lowers BS – Insulin. Yes, we only have one major hormone to lower BS, compared to 5 that increase it. You can probably see that if Insulin isn’t working right, there’s a problem – elevated BS, which leads to all the problems associated with T2D discussed later.
So, how does Insulin stop working in T2D?
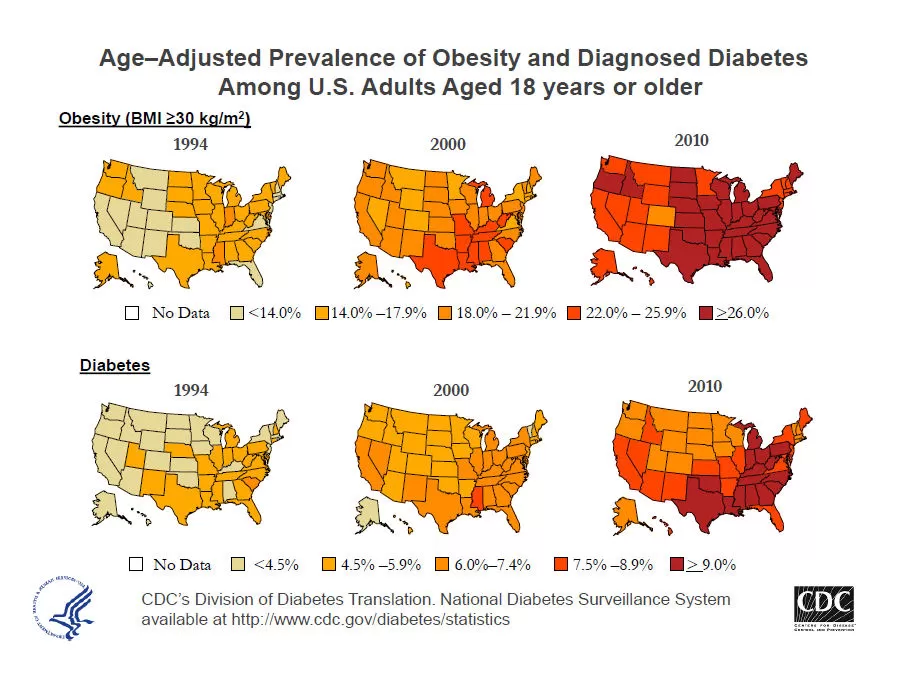
The first step occurs in food choices. If you eat a diet of processed foods (as opposed to whole foods) and don’t exercise much, then it is likely you are taking in more sugar than your body can use. Sugar, like high fructose corn syrup, is hidden in many processed foods. All carbohydrates (90+%), when digested – with the exception of fiber – turn into sugar and are absorbed affecting BS. So a situation is developing where you are taking in more sugar than your cells (primarily your muscle cells because they make up the largest metabolically active group of cells in your body) can use. Insulin works to drive glucose into your cells for use and is released when the BS increases after a meal. The more sugar absorbed, the more Insulin released. If your muscle cells are full of sugar and don’t need any more – as is the case when you consistently eat more carbohydrate than your muscles need and can burn – they resist the effects of Insulin and are then said to be Insulin Resistant. This is the first step in the development of T2D – Insulin resistance of the muscle cells. And if you get little exercise, your muscle cells need less sugar to power them. With less exercise, your muscles grow smaller and therefore need even less energy (sugar) to power them. And because your muscles run off fat as well, the more fat stores you have in your body, the less sugar your muscles use for energy. as a matter of fact, at rest your muscles (including your heart) get most of their energy from burning fat. It is only during exercise that your muscles burn mostly sugar. Each of these factors add to muscle’s Insulin Resistance (IR) as you continue to take in the same amounts of sugar (non-fibrous carbohydrate).
Once your muscle cells have become Insulin Resistant, where does the sugar go?
Your liver and fat cells remain Sensitive to Insulin and are said to be Insulin Sensitive. So, the Insulin causes a small amount of glucose to go into your fat cells to supply energy needs, but fat cells have low energy needs, being mainly storage depots for fat. So now the majority of BS is taken up by your liver cells where it is converted primarily into Triglycerides (TG) – the main storage form of fat – and some into Cholesterol (C). Both your TG and C are sent back out into the blood to be transferred to your fat cells for storage. Your Insulin also causes fat cells to take up TG and C (another one of Insulin’s functions) where they are stored because your fat cells are still Insulin Sensitive (IS). It is important to recognize that even with all this abnormal metabolism going on, at this stage your BS, TG & C blood levels are still normal because your BS is removed from the blood and turned into TG & C and these are removed from the blood by Insulin and stored into your fat cells. This maintains normal levels of each. At this stage you gain weight and without a change in lifestyle or food choices, continue gaining weight becoming overweight or obese. With a change from processed foods to whole foods and improved exercise, this stage can be reversed. The earlier you catch it, the easier it is to reverse.
The next stage in the development of T2D occurs when your fat cells become Insulin Resistant (IR). We don’t yet understand why some people’s fat cells become IR and others don’t. Some people’s fat cells remain Insulin Sensitive and they just keep gaining weight, developing severe obesity. But it is more likely your fat cells become IR and at this stage the TG & C produced in the liver, as you continue to consume the same amount of carbohydrates, have no place to go. Since your liver always stays Insulin Sensitive (IS), your BS will continue to be converted to TG & C and this is the stage when these blood levels of TG & C begin to increase. Your liver continues to produce them from continued over-consumption of carbohydrates and your doctor likely puts you on a lipid lowering medication (statins and fibrates are examples) to lower them. Many of these drugs work by preventing the conversion of BS to TG & C. Now the excess sugar has no where to go, so this then causes the back-up of sugar in your blood. Your BS begins to rise. This is why one of the side effects of these medications is that they cause T2D. (Please do not stop a medication without consulting a doctor for your own safety.)
Not only do your fat cells need to be Insulin Sensitive to take up TG & C, but also to hold on to the stored TG. When your fat cells are IR, they begin to leak the smaller components of the TG stored in them. These smaller components – Free Fatty Acids (FFA) – begin to rise in your blood along with the TG & C levels. The elevated Free Fatty Acids (FFA) are toxic to the pancreas and so begin to damage your cells that produce Insulin. This damage tends to take time and so your BS at this stage is still normal since your BS is still being converted to TG & C by your liver (as long as you haven’t been put on a medication to prevent the conversion (statin & fibrates). At some point between the IR of your muscle and fat cells but before significant damage to the pancreas, Insulin production goes up in an effort to overcome the IR of these two cell groups and it is here that your insulin levels become elevated. During this time, if your doctor has missed the weight gain and your elevated TG &C as indicators of your progression towards T2D, he/she may be able to pick it up by measuring your fasting insulin.
The last stage occurs when there has been sufficient damage to your pancreas from the leaking FFA that it can no longer produce enough insulin to force the liver to convert all the BS to TG & C. At this stage your BS begins to rise. At first it only goes up right after you eat. Then, after more pancreatic damage has occurred, your blood sugar stays high between meals. And lastly, after even more damage to your pancrease, your BS stays high throughout the night and into the morning before you eat – i.e. after fasting overnight. This means that in this process of developing T2D the Fasting Blood Sugar (FBS) is the last test to become positive. And this is the test most doctors use to determine if you are developing Diabetes. As a matter of fact, the definition of Diabetes Mellitus is a FBS > 126. As you can see, at this point the Genie is already out of the bottle! The damage to your pancreas has already occurred! At this stage, since not all your BS is being converted to TG & C, your TG & C levels may drop a little and you may even lose a little weight. If you didn’t know your BS was elevating and insulin decreasing from pancreatic damage, you might think this was a good thing, but it’s not because the reasons for it happening are increasing damage and disease progression.
How do the Counter-Regulatory Hormones contribute?
Stress is a major contributor. Stress causes elevation of your Cortisol, Adrenalin & Norepinephrine. All 3 of these hormones cause the breakdown of the protein in your body and the production of more sugar from that protein. The majority of protein is located in your muscles and so over prolonged periods of stress there is muscle wasting and you have less need for sugar for energy. The broken down proteins are used by these hormones to make more sugar that raises your BS even more. And when people are stressed, they often crave carbohydrates, compounding the problem. Also, many people ascribe to high protein diets to treat T2D. But if you eat a high protein and low carbohydrate diet, you turn on Glucagon (another counter-regulatory hormone) and worsen Insulin Resistance. This happens because Insulin is required to make protein go into muscle cells, but if your muscle cells are already Insulin Resistant, this can’t happen very well. The excess protein from these high protein diets then cause the secretion of Glucagon, which converts these high protein diet proteins into sugar since they have no other place to go, which increases BS. With higher blood sugar, you increase your Insulin Resistance.
What about other hormones, do they play a role?
Both Testosterone and Estrogen are anabolic hormones. They cause muscle to grow. Increased muscle means you burn more energy – both sugar and fat. This is why after menopause and andropause most people begin to gain weight. Progesterone also plays a role blood sugar metabolism. From a health standpoint, this is an important reason for bio-identical hormone replacement.
“Is it too late once I have T2D?”
First, let me say it’s never too late. It isn’t over till it’s over! Much of the time the entire process can be completely reversed. It depends on how much damage has been done to your pancreas, how much of that damage can be reversed, and how much pancreatic reserve you have relative to what and how you eat. There are many consequences of long term T2D including: Chronic Fatigue, High Blood Pressure, Heart Disease, MI, Stroke, Peripheral Vascular disease, Loss of Limb, Peripheral Neuropathy, Diabetic Retinopathy, Blindness and many more. If any of these secondary conditions have developed, correcting the underlying diabetes or secondary condition (the list above) may not be completely possible, but healthier food choices, lifestyle and proper nutritional supplementation must be considered the primary solution since they were the cause of the problem in the first place. Additional medication may be necessary to prevent further damage as lifestyle and proper nutrition are instituted. In the short term, IV nutrition may help because studies show that when you are overweight you have high risk of micronutrient deficiency (malnutrition), inflammation and oxidative stress, which all contribute to the development of T2D. To be lasting, lifestyle changes generally take time and personal patience. Once implemented, you and your doctor may find you need less medication or no medication at all and that your T2D, as well, as your secondary health condition has stabilized or reversed.
“I don’t have T2D but I am overweight so I can see that I am at risk. What can I do?”
If you begin eating primarily whole foods and few processed foods, exercise, don’t smoke and reduce stress, the likelihood of developing T2D is minimal and you will likely lose weight. These answers are simple but not easy. There are a variety of articles on my website designed to help you. Watch the movies listed in my article: “Documentaries on Food and Health”. Educate yourself on real health. Initiate small steps. You absolutely can make healthy choices and healthy changes.
If you have any questions or want help, please call Dr. Cole at one of our 3 locations in South Pinellas (727) 202-6807, Mid-Pinellas (727) 518-9808 or North Pinellas (727) 786-1661.


0 Comments